Electronic Patient Record - Home Treatment Team SBAR
Product Design Team - Surrey and Borders Partnership NHS Foundation Trust
Brief
Improve the handover practice for Home Treatment Teams using SBAR (Situation, Background, Assessment and Recommendation) integration into the Electronic Health Record.
Digital teams are to work collaboratively along side the Clinical Teams to improve and optimise the handover practice of our Home Treatment Teams. Shifts work to cover 24/7.
SBAR (Situation, Background, Assessment and Recommendation) Is a well established communication tool within the NHS.
The original SBAR process was done in Excel before we did this project.
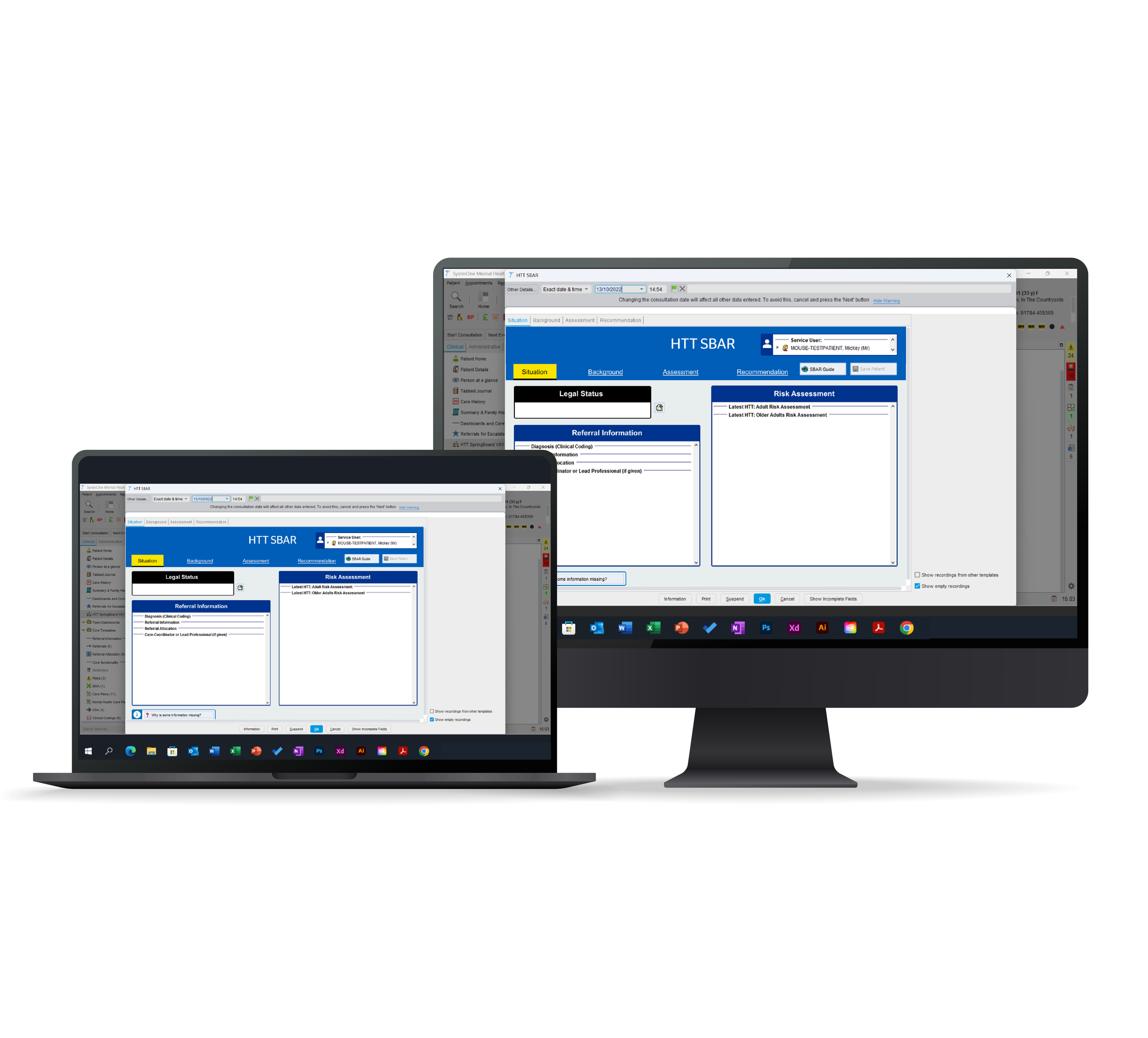
This is the demo EPR and ONLY uses test patients, not live/real patient data.
Our Trust uses SystmOne (Electronic patient record software) created by TPP for the NHS. Our Teams work using Agile Scrum and User Centred Design.
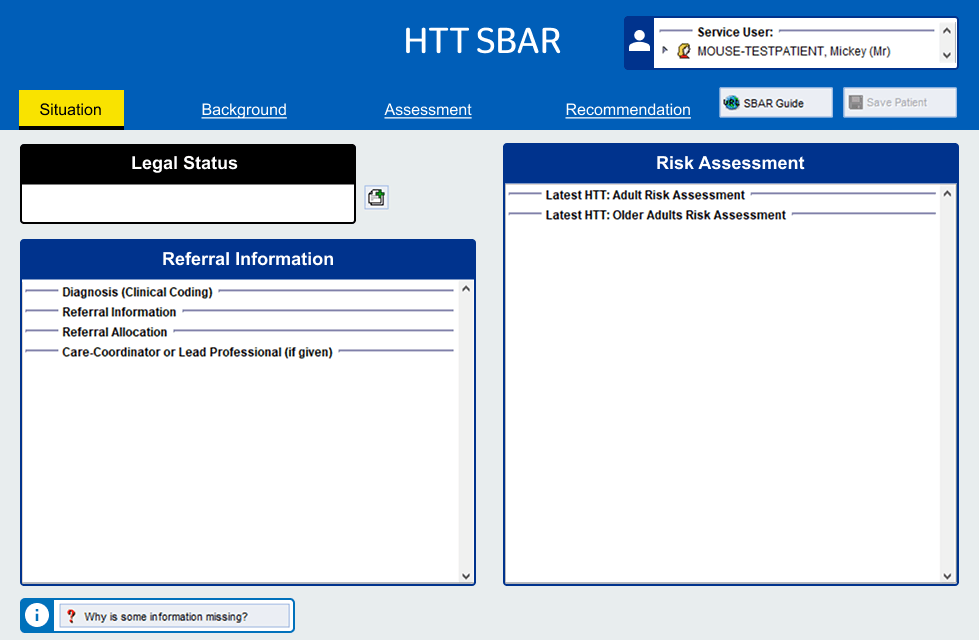
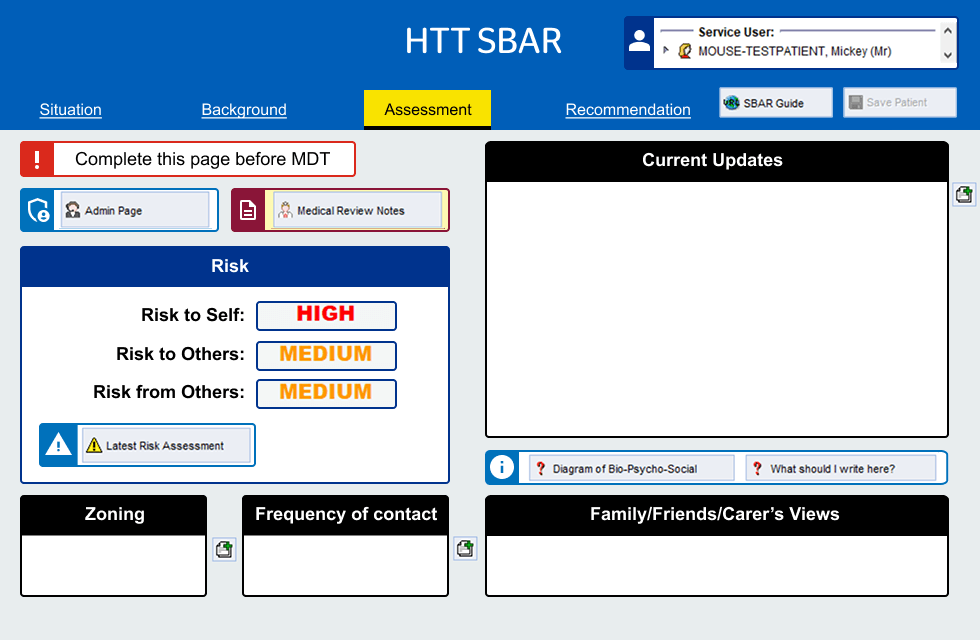
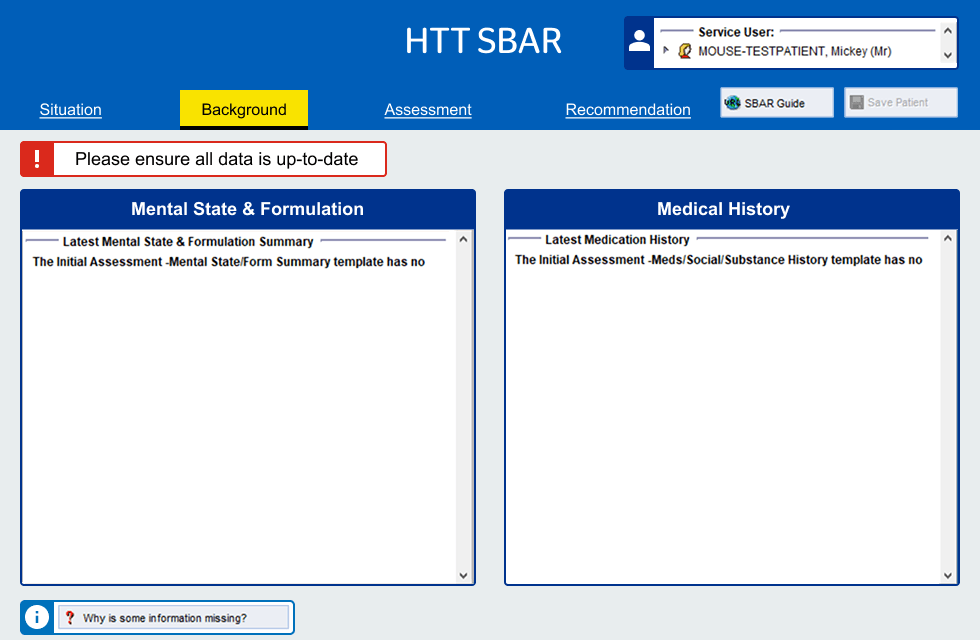
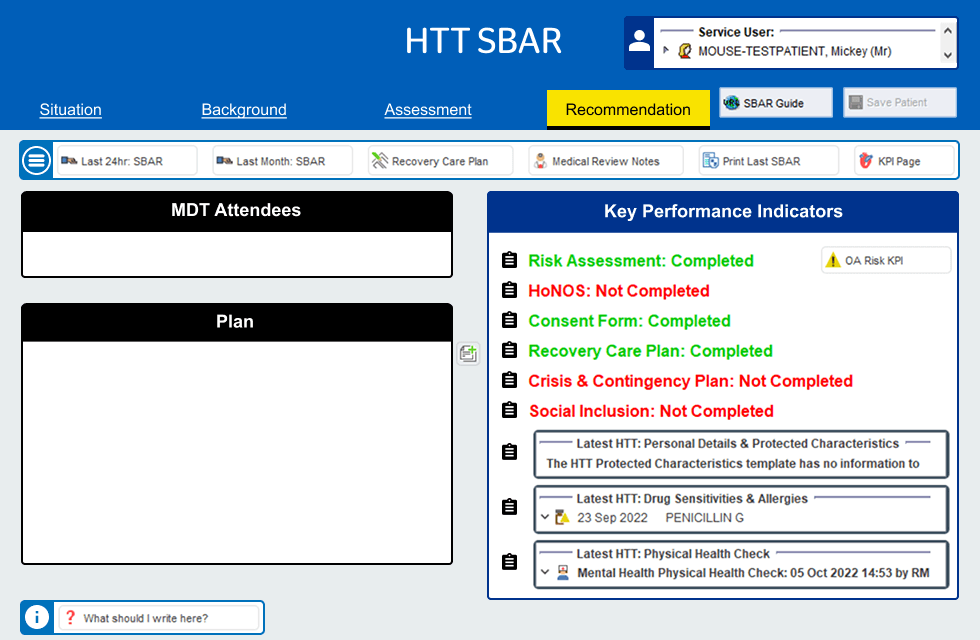
Above: HTT SBAR in the Demo Electronic Patient Record (SystmOne TPP) with a test / dummy patient. (NHS Logo is removed for online display of work)
Project Goals
Replicate NHS SBAR best practice digitally (directly into the Electronic patient record)
Implement the SBAR in SystmOne EPR
Conduct a User friendly re-design tailoring it for HTT needs
Reduce the time of handover meetings, Less time on manual data entry
Ensure no overtime required by the Administrators
Maintain a high level of patient care
Business goal: is to reduce the reliance on word documents and make better use of our electronic patient record system (SystmOne)
Reduce errors
Working towards single source of truth for patient data
Better patient outcomes due to more time available for patient care
Safer storage of information
Challenges
Some technical limitations to make changes to the EPR software, SystmOne
Working to tight deadlines to meet frontline service needs
Clinical staff availability is limited to do testing and plan workshops
Project Team and my involvement in the project
Immediate Team: (Design Team Flow) Product Owner, 2X UX Researchers, 3 UX Designers, Scrum Master
Wider Teams: Learning and Adoption team, App Support team.
Primary users: Admin Staff. East & Mid HTT Staff (for initial role out), all other HTT staff who attend the MDT meeting
Secondary users: Could be extended to HTTs from other directorates and ISS.
Stakeholders: Associate director Working Age Adults and Inpatients, Associate Director of Flow and Bed Optimisation, Associate Director of Digital Transformation Delivery. Head of Home Treatment Teams East and Mid Surrey.
My Involvement in the project:
I supported the UX researchers in Discovery. I designed the Usability testing plan and designed the tests for Qualitative Usability testing.
I did iterations of the High Fidelity working prototype in the EPR. I designed the user testing plan and designed the tests for Qualitative usability testing.
Skills & Software
UX Research
UX Design
UI Design
Prototypes
Usability testing
Miro
Adobe XD
Workshops
Discovery - Contextual Studies & Personas
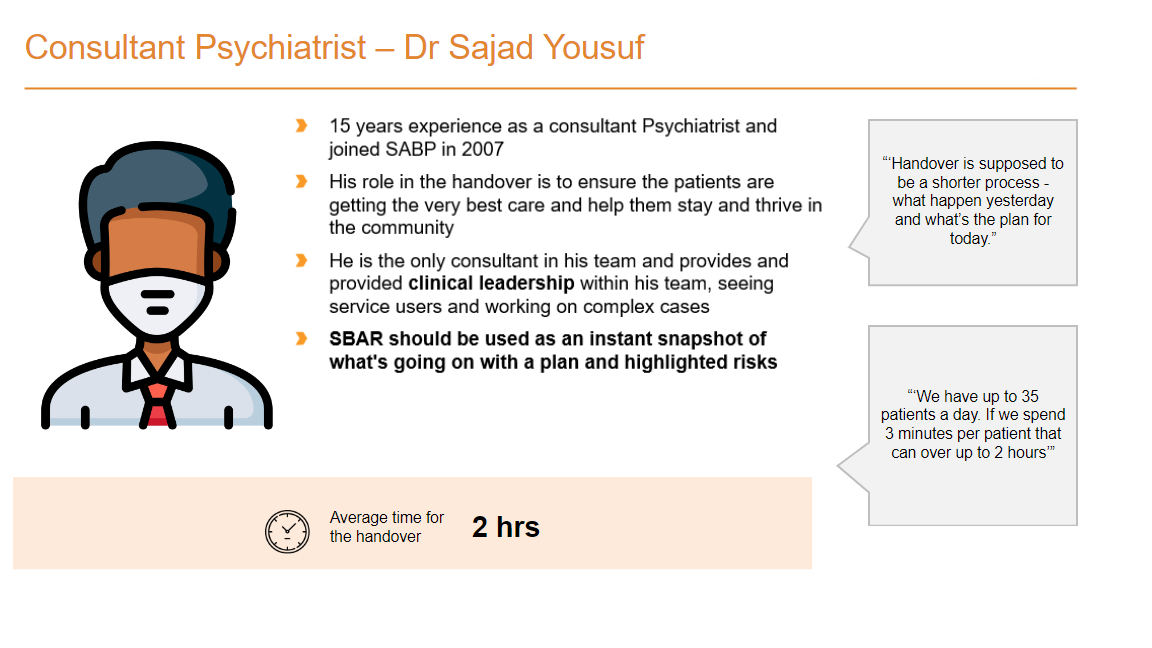
Personas were created from on site contextual interviews at NHS SABP East and Mid HTT base (Redhill Surrey). Visits were UX Researchers and UX Designers.
Above: Insights and Pain points Consultant Psychiatrist
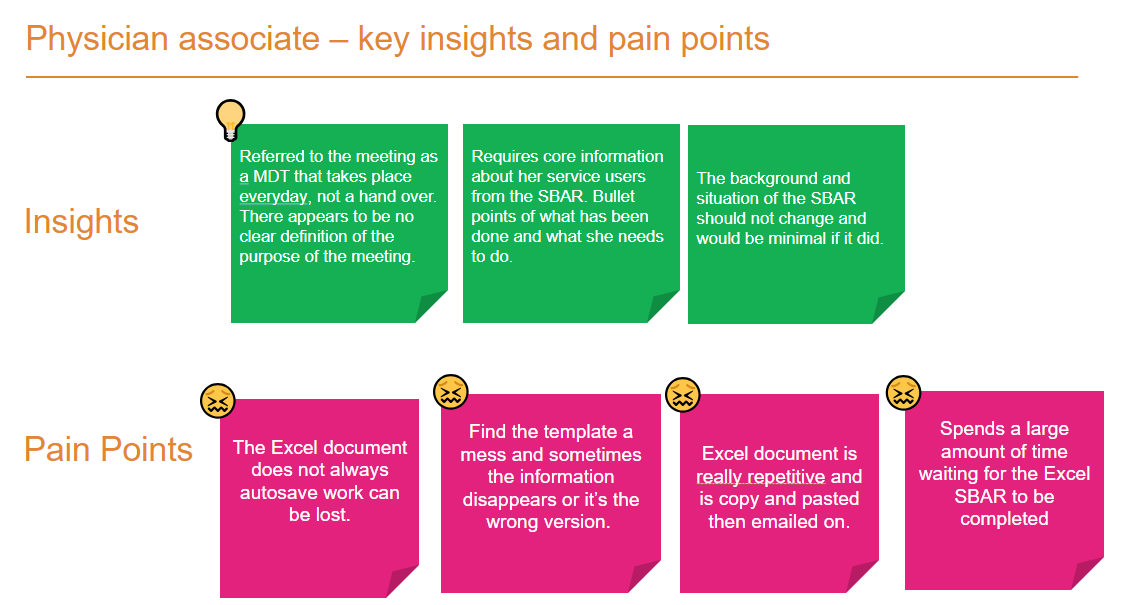
Above: Persona for Primary user Physician associate
Above: Insights and Pain points Physician associate
Recommendations and thoughts from the Interview
Pre-population of situation and background
Move away from updating and sharing Excel documents
What had been clear during the research is that there appears to be consensus that the handover has become more of an MDT meeting
Possibility of out of Scope for digital, but looking and having a '“stand up” during the handover
Can the information be pulled from SystmOne (Electronic patient Record) to reduce any duplication and Repetitiveness?
Can the allocation of service users be done before Hand over?
A paper version(prototype) has been shared with the design team. This should be tested
The SBAR should be an instant snapshot of the service user
We feel the Home treatment team would benefit from having some service design or QI support
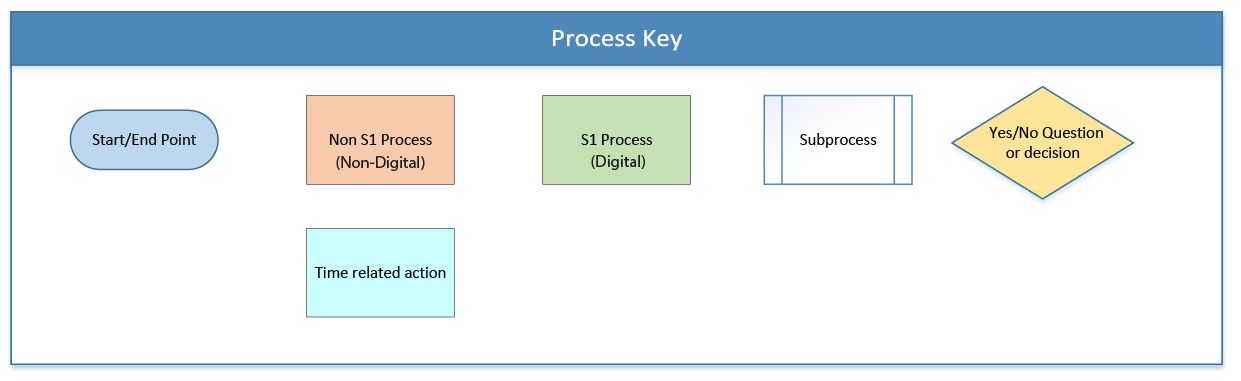
Alpha Phase - To Be Process Map
This is the proposed To Be Process map of the service showing both online and offline processes.
Above: To Be Process map for the HTT SBAR, Please select this text to view larger image
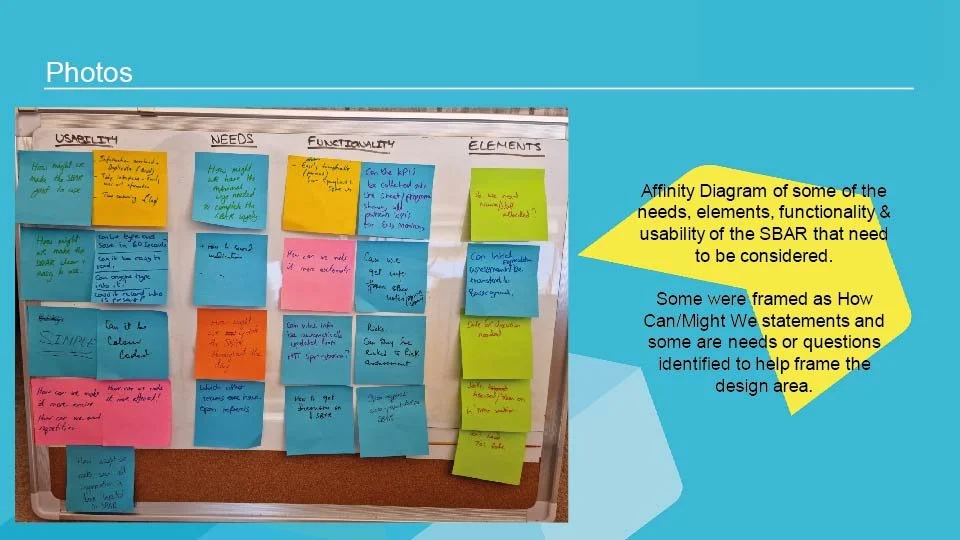
Alpha Phase - Co Design workshop
The Co Design Workshops took place on site.
Please see full PDF here: HTT Co Design Workshop plan
Above: First Co Design Workshop PDF
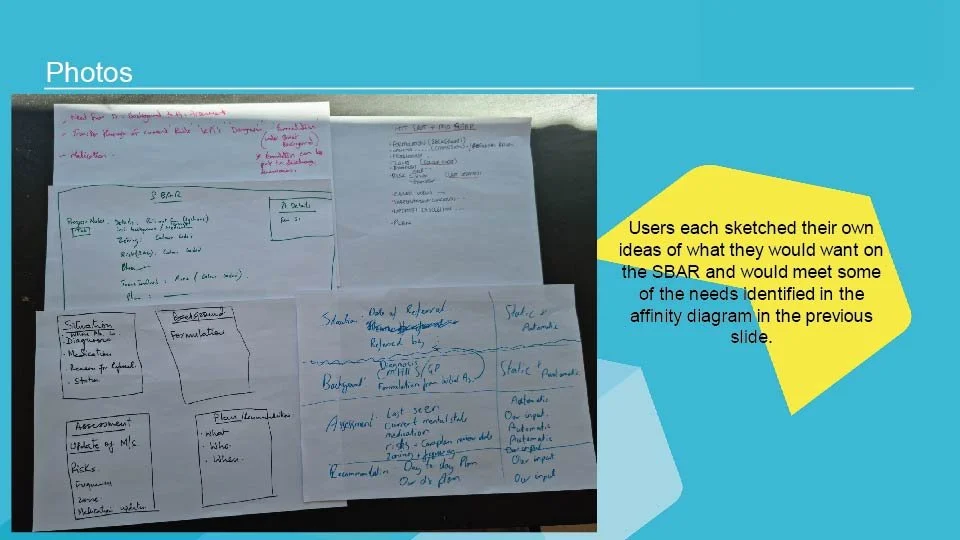
Above: User sketches from the Co Design workshop
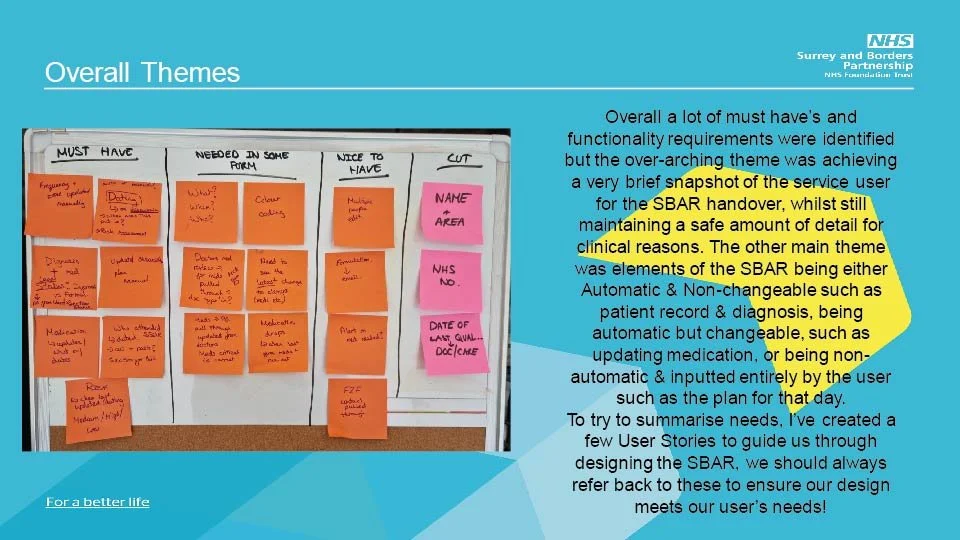
Above: This is example is using a MoSCoW prioritization. The acronym MoSCoW represents four categories of initiatives: must-have, should-have, could-have, and won't-have, or will not have right now.
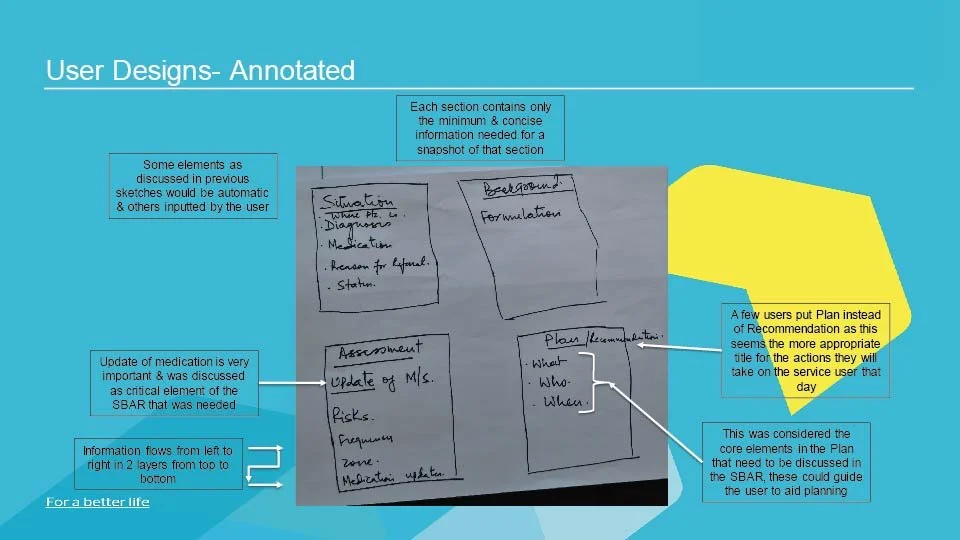
Above: Annotated user sketches. These sketches will inform the low fi prototype
Alpha Phase - Low Fi Prototype (shown in the 2nd Co Design / Critique workshop)
The Low Fi Designs were taken to the 2nd Co Design Workshop and iterated after that
I also created the ‘TO BE’ Process maps (multiple versions) from the ‘AS IS’ process map the UX Researchers did.
Above: Lo Fi Situation & Background page (combine on to one page in this early iteration)
Above: Lo Fi Plan (Recommendation page)
Above: Assessment page (combine on to one page in this early iteration)
Alpha Phase - Usability Testing
A High Fidelity working prototype was created in SystmOne to do Usability testing with, using test patient data (no real data was used), iterations were made from 2nd co design workshop.
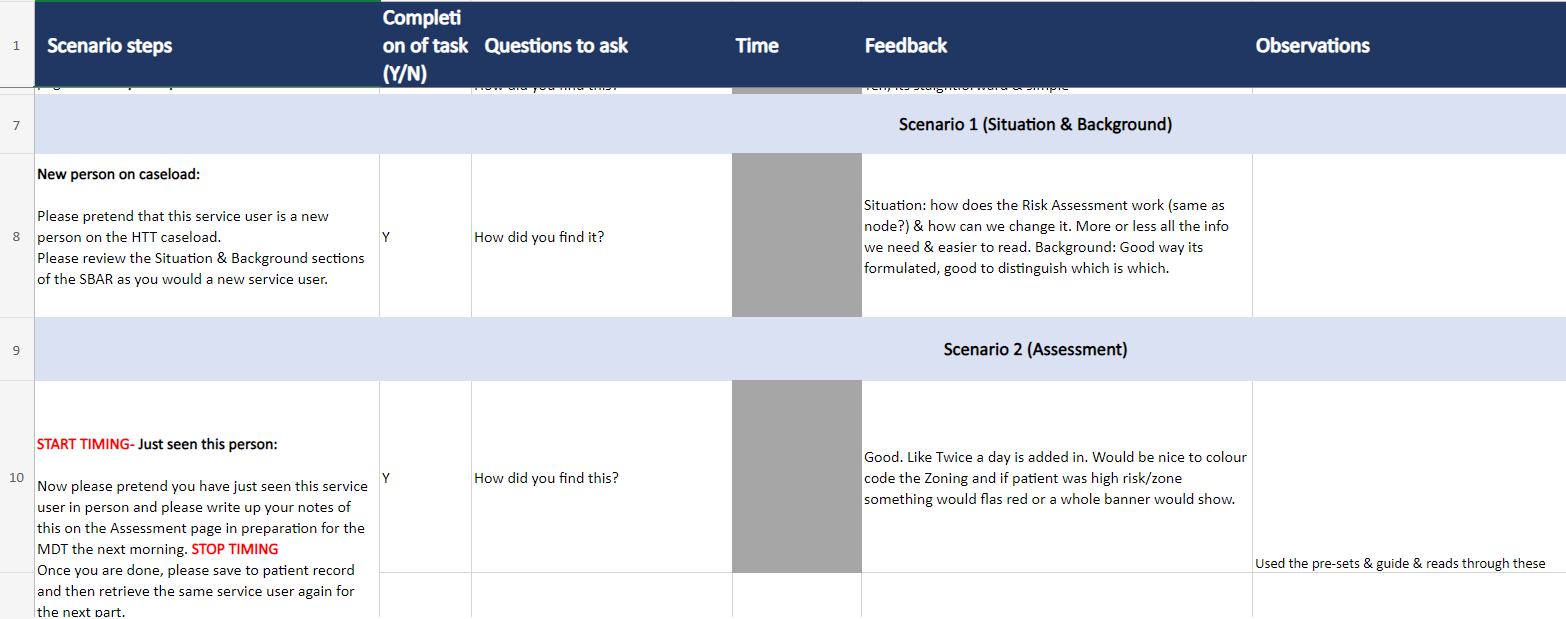
I designed the Usability Tests (plan and scenario questions), we did two rounds.
Myself and another UX designer working on the project went on site to do two round of Moderated Usability Testing
Purpose: Test the outcomes from Co Design Workshops by Usability testing a Higher Fidelity working prototype (in the EPR)
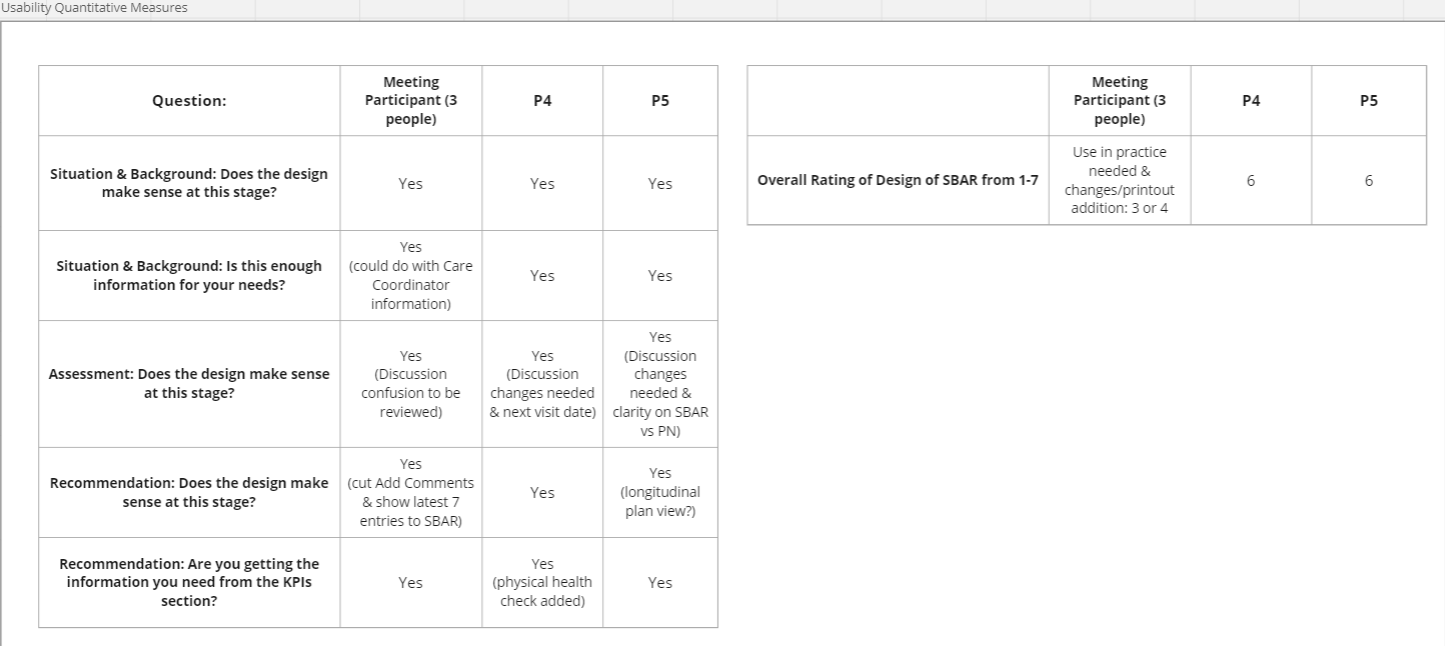
Above: Round 1 Usability Quantitative Measures (task completion) - put on Miro
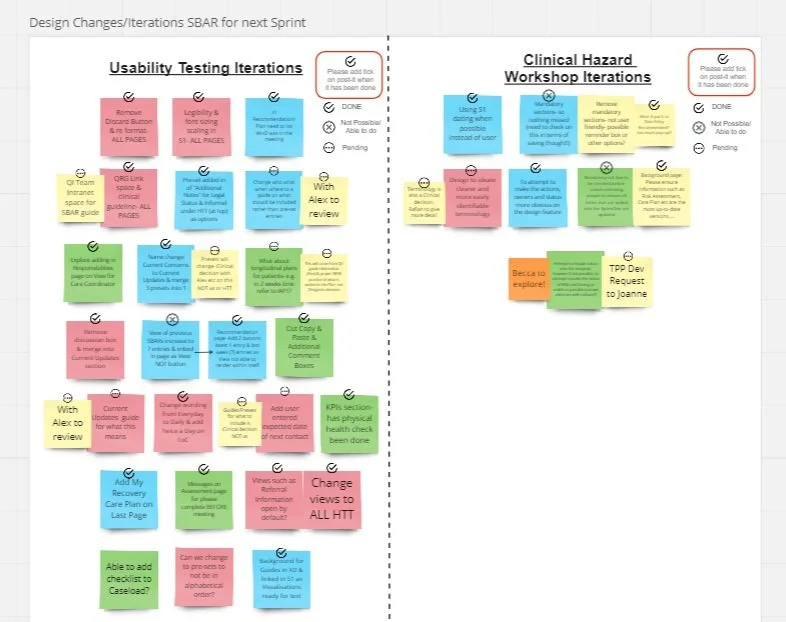
Above: Iterations for prototype from Round 1 and Clinical Hazard workshop
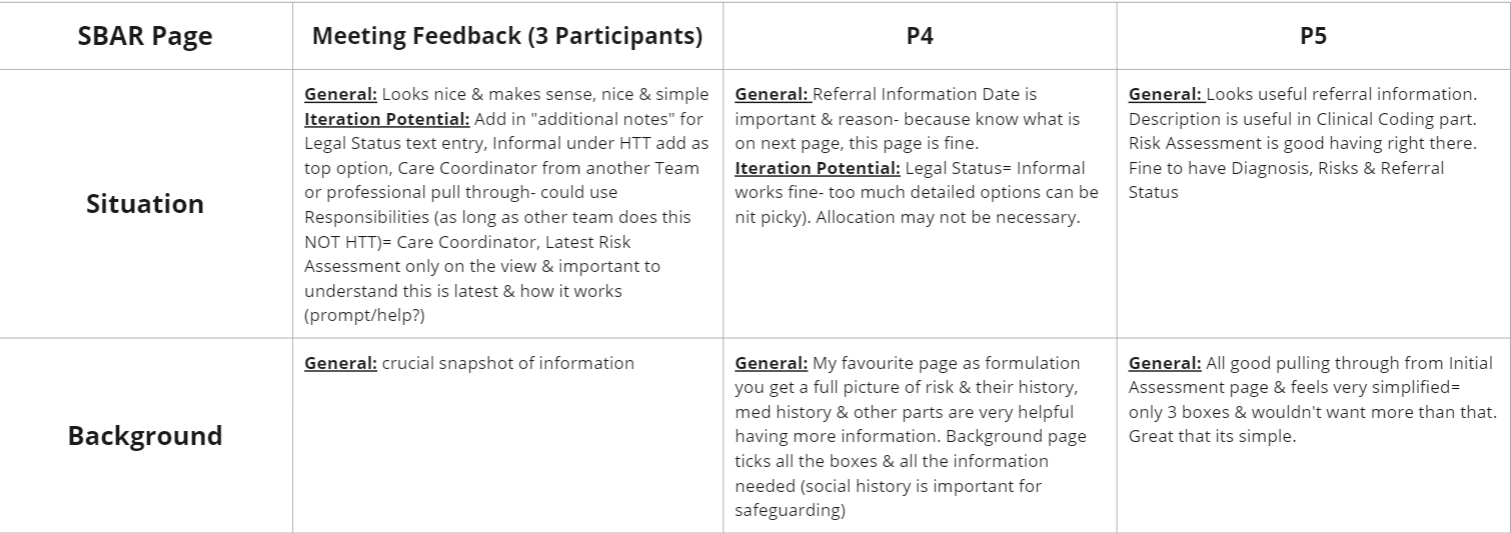
Above: Usability Qualitative measures - User feedback put on Miro from Excel Doc, Round1
Above: Usability test scenario questions from Excel round 2
Above: Usability Qualitative measures - User feedback put on Miro from Excel Doc, Round 1
Above: Iterations for prototype from round 2 on Miro
Alpha Phase - High Fi Prototype
These Designs are built in System One (TPP) An Electronic Patient Record that many NHS Trusts use across the country.
Please note: There were some restrictions creating the working prototypes in SystemOne, and some colours are not accessible and we have no control over this.
The dimensions were 980 x 650 px, and the software isn’t responsive to screen size.
These are the dimensions that would fit on a laptop screen.
NHS Logo is removed for online display of work.
Above: High Fi working prototype in SystemOne, Situation page
Above: High Fi working prototype in SystemOne, Assessment page
Above: High Fi working prototype in SystemOne, Background page
Above: High Fi working prototype in SystemOne, Recommendation page
Beta Phase - UAT
UAT was done remotely via Teams with minor changes
Very little needed to be fixed because we had involved the user in the process end to end (Alpha phase Co-design and Usability testing caught issues early on and we could address them)
Throughout the process we had kept checking the User Stories against our designs and prototypes
UAT should be for testing for bugs and technical issues.
Beta Phase - Pilot outcomes
Our intended measures of success were gathered during the month long pilot of the SBAR with East and Mid Surrey.
Measures of Success:
Staff Satisfaction
Timing of MDTs
Need for overtime by Administrators
Financial Impact
Quality of Patient care
During the Pilot, support was given by Flow design team, QI, Applications Support and Learning and Adoption Teams as well as the Clinical Lead for HTT.
In terms of evidence of achieved targets:
The MDT reduced by 30-60 mins on average which for just one HTT team equates to 3,500 hours of clinical time saved, meaning staff have more time to prioritise patient care. Time Saved in Hours: 17,264 for 4 teams.
Financial predictions from the QI team put this at a yearly cost saving of 160k for just One HTT (4 teams in total so 640k )
Admin save 8k a year on overtime costs
Significant financial savings as the MDT/handover is, on average, 30-60 minutes shorter.
86% of staff now only update the plan for that day during the MDT (as opposed to multiple times a day). An organised and streamlined MDT/handover.
Staff satisfaction with the design was measure through surveys with multiple staff saying it was:
“Much Quicker”
“Easy to Use”
“Improved Quality of conversation during MDT”
“Removed a load off the shoulder of Admin”
Please note: The quality of patient care will be better because of the Clinicians’ time saved
Results -
Money: Saved 640k (over 4 teams in total) per year
Time Saved in Hours: 17,264 per year
Nominated for Health Service Journal Awards 2023
Category : Replicating Digital Best Practice Award Finalist
https://digitalawards.hsj.co.uk/winners-2023Better patient care from the Clincians’ time saved
See more examples and case studies:
For more choices, please continue to browse my portfolio or use the navigation below.